After a shock diagnosis of bowel cancer, Bernadette now wants to educate everyone about testing and early diagnosis
- Home
- Patient News
- After a shock diagnosis of bowel cancer, Bernadette now wants to educate everyone about testing and
June was Bowel Cancer Awareness Month. The number of people diagnosed is stark and confronting, but bowel cancer is also one of the most treatable conditions if detected early. St Vincent’s Private Hospital Northside puts a spotlight on the issue.
The numbers are stark and confronting. Each year over 15,000 Australians are diagnosed with bowel cancer – 300 each week including almost 1,700 people (one in 10) who are under the age of 50. It is the third most commonly diagnosed cancer and the second deadliest cancer after lung cancer. Around 5,000 people die each year from bowel cancer.
One of St Vincent’s colorectal surgeons, Professor David Clark, says it’s a remarkable situation where you have a cancer that is so important to diagnose early, yet many people don’t take up the simple screening test. This test is distributed free by the Federal Government to the at-risk population.
He says across Australia, around the world in Westernised countries and in his own medical practice at St Vincent’s Private Hospital Northside, he’s seeing increasing numbers of young people diagnosed with bowel cancer and the number of patients younger than 40 is increasing.

Professor Clark says the reasons for more bowel cancer diagnoses are somewhat unclear and there is insufficient data to provide provable links. Experts understand that the important risk factors are related to diet (including red meat consumption), low physical activity, obesity, alcohol and smoking as well as family history.
“Unfortunately for many young patients, minor symptoms are often attributed to common benign conditions and not immediately investigated. This will see a loss of opportunity to have curative surgery,” said Professor Clark.
People aged 50-74 years remain the highest risk group. A simple stool test is distributed free under the federally funded National Bowel Cancer Screening program. Given the rise in incidence among younger Australians, there’s a push to have the program extended to increase screening from age 40.
National peak body, the Gastroenterological Society of Australia (GESA), aims to review the Australian and international data to assess whether it should recommend to the Federal Government that the age for free screening should be maintained or lowered to 45 or possibly even 40.
Professor Ben Devereaux is president of GESA as well as a gastroenterologist with experience in therapeutic endoscopy and pancreatology at St Vincent’s Private Hospital Northside.
“Preliminary reviews of the data seem to indicate that we are seeing more cases of bowel cancer in people under 50, so it’s timely for us to be reviewing it,” Professor Devereaux said.
Professor Devereaux and Professor Clark are mindful that if the free screening age was lowered, there would be an additional financial cost to the health system in the short term, but this would be outweighed by the community benefit and many young lives would be saved.

The story of 54-year-old Brisbane mother and teacher Bernadette Toohey is a cautionary tale for everyone. She had no symptoms of bowel cancer and no family history.
But last June, she followed her GPs advice and (finally, she says) did the free bowel cancer screening test which she had previously left sitting in a drawer. After a positive result she went on to have a colonoscopy.
The Physical Education teacher says she was “overwhelmed, shocked and in disbelief” to learn she had stage three bowel cancer which required urgent surgery by St Vincent's Northside Professor David Clark.
“One moment I was living a happy, normal life and next thing I know I am trying to comprehend being told that not only did I have cancer, but it was already stage three and required major surgery. Fortunately, I am generally a positive person so straight away I asked my specialist, “Okay, so what’s the next step? How do we deal with this type of cancer?”

Following her diagnosis, the next few hours were a blur as Bernie immediately underwent further tests at the hospital that day and later left St Vincent’s Northside already booked in for surgery the following week. The hardest part of her diagnosis Bernie says was going home and sharing the unexpected and concerning news with her two daughters and immediate family.
“Thankfully I had the company and support of my incredible husband by my side when I received the life-changing news and he has been a constant source of strength and positivity for myself and our girls each day since,” says Bernie.
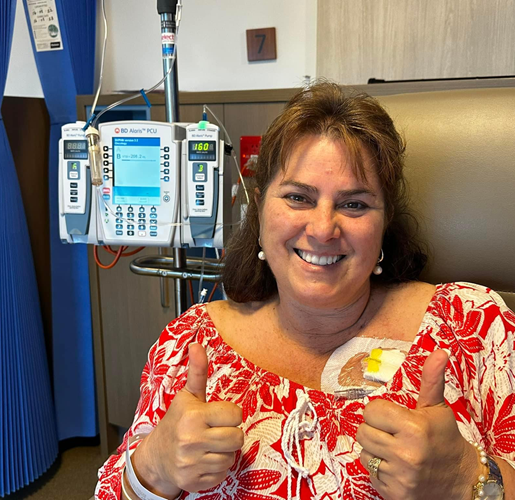
Immediately after her colorectal surgery, Bernie followed the advice of St Vincent’s Northside oncologist Dr Rick Abraham and underwent six months of chemotherapy, visiting the hospital Oncology Department each fortnight.
She initially took three months off her teaching job while she started treatment to see how her body would cope and to give herself the best possible chance of recovery.
In the second half of her treatment, Bernie was fortunate to be well enough and able to return to part time teaching – and is appreciative of her understanding employers and incredibly supportive network of family and friends.
“I’m the type of person who takes their health seriously and prioritises it with annual health checks – also being a Physical Education teacher makes you aware of the importance of looking after the only body you’ve got,” says Bernie.
“I don’t drink or smoke, I’m active and try to watch what I eat. But you can’t tell from the outside what your health is really like on the inside so taking advantage of free bowel screening, especially if you’re over 50, is a simple way to know what’s going on inside your body.”
There was no obvious trigger or reason for her bowel cancer diagnosis – fortunately Bernie recently received a clean bill of health and considers herself one of the ‘lucky ones’. While she had 17cm of her bowel and lymph nodes removed she says she is grateful that doctors detected it early enough to treat her with favourable outcomes.
She’s thankful that she and her doctors were vigilant about the free bowel screening and follow-up colonoscopy and has since learnt that if the cancer cells had gone undetected for another 12 months, it may have been a 'death sentence.'
According to Bernie: “I feel blessed that I had such a high-quality team of medical professionals looking after me. Everyone at St Vincent’s was amazing and very compassionate – I am indebted to all the doctors, as well as the fabulous staff and volunteers at St Vincent’s Hospital Northside”.
Feeling grateful for such a positive health outcome since her diagnosis, Bernie says she was happy to take up the challenge put to her by Dr Clark, to be an active voice and ‘walking/talking billboard’ to promote the importance of the national bowel screening program.
She is sharing her cancer story with her friends, family, and school community and Bernie’s message is clear, urging everyone aged over 50 to take the free screening test and help raise awareness in the younger adult population. As a previous recipient of the ACHPERUQ (Australian Council for Health, Physical Education and Recreation Queensland Branch) Inspirational PE Teacher of the Year Award, Bernie understands the benefits of being a positive role model and is using her personal experience (with her school's permission), to educate her students and getting them to be a reminder to their parents about the test!
“I’ve had dozens of my friends and colleagues who have been motivated to do the test since I was diagnosed and thankfully they’ve got the all clear. Since sharing my cancer journey I’ve also had many parents and staff members at my school reach out and thank me for raising awareness in their families and offering such positivity,” she says.

Professor Clark also recommended that people undergo further examination with their GP at the first sign of symptoms – which could either be blood in their stool or change in bowel habit, no matter what their age.
Bleeding was the most common symptom – it is also often associated with haemorrhoids – but it can also often be a sign that that the issue is starting to progress towards the cancer stage or cancer is possibly already present.
Professor Clark is involved in several collaborative studies supported by St Vincent’s Hospital Northside and the Queensland Institute of Medical Research which are focussing on personalised therapy and future treatment paradigms.
Colorectal cancer cells are ‘able to hide’ from the immune system and one project is looking to enhance the immune system to ‘revisualise’ these abnormal cancer cells with the goal to enable the immune system to perform its normal job of killing cancer cells.
Another exciting project is designed to use cancer cells from a patient to grow cancer organoids in the laboratory that will enable specific testing of therapies and then verify the most effective treatment on those cells.
Professor Clark says this personalised or tailored therapy is the future of cancer treatment.




