Breast implants have been in existence for a few decades now. Celebrities such as Dolly Parton and Pamela Anderson are considered early adopters of breast implants when their use was rather obvious to the casual observer. Over time, however, Plastic Surgeons and implant companies have made progress in getting implants to look and feel more natural.
Implants find uses in various contexts:
- Cosmetic: where smaller-breasted women want to have an increased breast volume, simply to improve their appearance
- Symmetrisation of developmental asymmetry: where an implant is able to offset any significant developmental asymmetry that a woman may experience through puberty
- Reconstruction: where a case of trauma or cancer may require a significant portion of the breast to be removed, an implant may be used to recreate the breast volume to maintain symmetry and cosmesis
Currently, the breast implant industry is worth US$1.5Bn a year, and it is expected to continue to grow over time. Typically constructed using a silicone or polyurethane shell, implants either contain silicone gel or saline to make up their volume. Both silicone and saline are considered inert and the TGA has approved both silicone and saline implants for use in Australia.
One of the positive features about implants, particular in the reconstructive setting, is their availability in a large range of sizes and shapes. Implants in Australia range from 100cc to 800cc (in the US, they may even exceed 1000cc) in volume. In terms of shape, the implants vary in terms of actual shape (round vs. anatomical “tear drop”), width, height, and projection. Implant shells can be smooth or textured, and silicone gel contents can vary in viscosity and “feel.” It is no surprise then that an implant manufacturer like Mentor lists 300 different types of implants in its catalogue.

Risks associated with breast Implants:
Capsular contracture: as a normal bodily process, a layer of scar tissue forms around the implant after it has been placed. This layer is known as the scar capsule. In most cases, the capsule does not pose any problems for women who have implants. In a number of cases, this capsule may thicken and contract around the implant, leading to distortion of implant/breast shape, feelings of tightness, decreased breast mobility, inability to take deep breaths of air, and possibly pain. This is known as capsular contracture. In the presence of pain from capsular contracture, the removal of the implant and capsule is recommended. The removal of the capsule is also known as a capsulectomy.
Implant rupture: implant shells are made of strong material and undergo rigorous laboratory testing to ensure integrity. However, the risk of implant rupture remains. Implant shells can weaken over time. In the past, implant manufacturers recommended that patients replace their implants after ten years. These days a replacement of implant is only recommended if complications arise. A rupture of a saline-filled implant is not considered as serious an issue as a rupture of a silicone-filled implant. That is because the saline is expected to be absorbed by the body without ill effect. Loose silicone in the body is a more complex situation. While inert, the effect of silicone uptake by the body is not fully understood. Silicone from a ruptured implant can be taken up by the lymph nodes. It is commonly agreed that where a rupture has occurred, the implants are removed with as much of the leaked content as possible.
BIA-ALCL: Breast Implant Associated Anaplastic Large Cell Lymphoma: BIA-ALCL is a type of lymphoma that can develop around breast implants. BIA-ALCL occurs most frequently in patients who have breast implants with textured surfaces. This is a cancer of the immune system, not a type of breast cancer. The current lifetime risk of BIA-ALCL is estimated to be 1:3,000 - 1:85,000 for women with textured implants. In the majority of cases, treating ALCL requires the removal of the implants with total capsulectomies and in a small number of cases, the addition of chemotherapy. The TGA has advised that if there are no signs or symptoms of ALCL, removal of the implants is not indicated.
Breast Implant Illness (“BII”): BII is the term used to describe a wide group of unexplained persisting symptoms that some women with breast implants experience. These symptoms may include aches and pain, chronic fatigue, brain fog, rashes, hair loss, and gastrointestinal discomfort. While studies are being conducted to understand the link between implants and these symptoms, the US FDA recently recognised BII as a risk associated with breast implants. A patient suspected of suffering from BII should first be assessed for other possible causes of the symptoms. These include autoimmune diseases (e.g. Lupus, Sjogren’s, rheumatoid arthritis, etc), tick-borne illnesses (e.g. Lyme), deficiencies (Vit D, folate, iron, etc.), and hypothyroidism. Most women with suspected BII report that most symptoms resolve after their implants and capsules are removed.
Removal of breast implants
There are a few different ways in which implants are commonly removed. They are listed below in ascending degrees of complexity:
- Implant removal only: this involves cutting open the scar capsule and removing the implant. The scar capsule is left in place.
- Implant removal and partial capsulectomy: this involves the excision of a part of the scar capsule (typically the superficial half) and the removal of the entire implant.
- Implant removal and full capsulectomy: this procedure is usually the removal of the superficial half of the scar capsule, followed by the removal of the implant, followed by the removal of the deeper half of the scar capsule. Usually, this leads to three items being removed per side (superficial half of capsule, implant, deep half of capsule)
- En-bloc implant removal and capsulectomy: this is the removal of the entire capsule as one whole piece, with the implant still contained within the capsule.
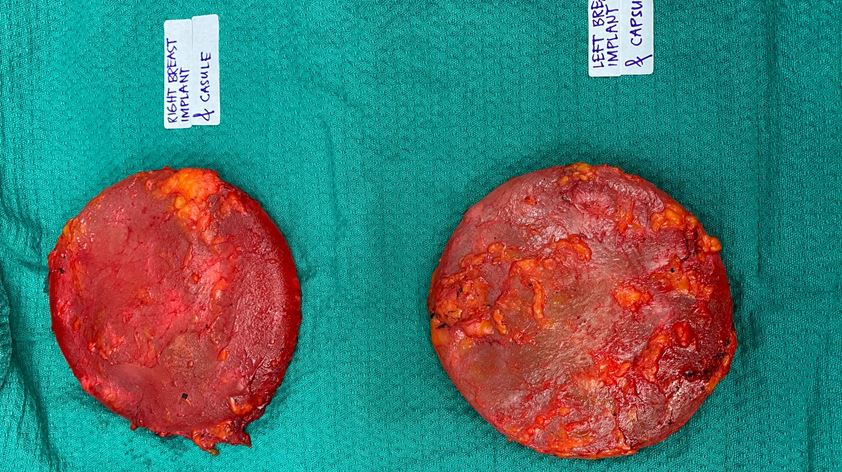
While most time-consuming, the en-bloc implant removal and capsulectomy is the preferred method of removal, especially where an implant rupture is suspected or confirmed. This method helps to ensure that implant content is fully removed from the chest cavity. Where implant silicone gel has leaked out of the capsule, the surgeon needs to take extra steps in removing the silicone from the site, and a complete removal of silicone is not guaranteed.
Interesting findings post explant
There are a few observations I have made related to explant surgery:
- For patients who report having systemic symptoms (“Breast Implant Illness”), there is typically a quick reduction in some of the symptoms they experience. A few persisting symptoms may take longer to resolve, if at all.
- Amongst the patients who have imaging performed on their implants and where no implant rupture is detected, about half of them will have trace quantities of silicone found (under microscope) on the scar capsule, indicating microscopic undetected leaks in the implant shell or disintegration of the shell itself.
- Patients who initially report having problems taking deep breaths of air (due to capsular contracture) usually find immediate relief from any restriction in breathing due to improvement in mechanics of breathing.
Adjusting attitudes towards implants and explants
Breast implants have their use, especially in the context of breast reconstruction or corrective surgery. While most women with breast implants do not encounter any complications with implants, it is crucial for surgeons to discuss the relevant risks of breast implants with their patients.
When I am approached by patients who are seeking breast implants purely for cosmetic reasons, I encourage them to extend their considerations beyond their perception of social norms and beauty and focus more on health. Equally though, there is at times a hesitation by women with implants to address problems they may be facing with implants. As practitioners, being aware and transparent about the use and risks of implants will help patients make more appropriate choices for themselves.
Specific to breast cancer, Breast Surgeons increasingly favour the use of breast conserving surgery (“lumpectomy”) instead of mastectomies wherever possible. The reconstruction options available to mastectomy patients are limited to implants or autologous reconstruction – both of which carry risks which would otherwise be avoided with breast conserving surgery.
Breast implants and routine breast screening
Women with breast implants should continue to undergo regular breast screening as per normal. While BreastScreen invites women aged 50 and over to undergo two-yearly screening (assuming no family history of breast or ovarian cancer), women may start screening with BreastScreen from the age of 40. Women with implants should highlight to BreastScreen/Radiology staff that they have breast implants so that adjustments can be made to the scans taken to allow for specific angles to be taken (“implant displacement views”).
About Dr Eva Nagy
Dr Eva Nagy is a Consultant Breast Surgeon. She sees and treats patients in Sydney’s North Shore and the Central Coast. While her focus is on the treatment of breast cancer and breast reconstruction, she also treats patients for benign conditions such as complications related to breast implants, and pain associated with macromastia.


