Thyroid Nodules
Thyroid nodules are a common finding, palpable in up to 7 percent of the general population and found incidentally in up to 60 percent of neck ultrasounds 1. Other common modalities where thyroid nodules are identified include carotid dopplers, CT, PET and MRI scans performed for other reasons. All thyroid nodules detected should undergo further workup.
Thyroid nodules should be assessed for the following:
- Hyperthyroidism
- Risk & Concern for malignancy
- Compressive symptoms
The workup of a thyroid nodule consists of a history for compressive symptoms, assessment of thyroid function and assessing the risk of malignancy.
History
Typical symptoms of compression such as difficulty breathing on exertion, difficulty lying supine and swallowing difficulty; may indicate possible mass effect by an enlarged thyroid nodule or nodules. Voice change is of significant concern as this may imply a malignant thyroid nodule is infiltrating the recurrent laryngeal nerve and this symptom should always be treated with a high index of suspicion. Other important features are a family history of thyroid carcinoma and exposure to radiation. Exposure to radiation such as external beam radiotherapy (EBRT) or nuclear accidents carries a risk of malignancy up to 40% in a patient with a thyroid nodule.
Thyroid Function Test
TSH should be tested in any patient with thyroid nodule(s) and if abnormal, T3 and T4 should be added. Thyroid malignancy typically does not produce additional hormone. If the TSH is low, a thyroid uptake scan should also be performed. If the uptake scan shows a single hot nodule, this is typically a single functioning adenoma; if multiple nodules show uptake, this indicates a toxic multinodular goitre. Hot nodules have a very low risk of malignancy and are typically not biopsied. Surgery is the most effective method of treating both toxic adenomas and toxic multinodular goitres. Other alternatives include RAI therapy which may require multiple treatment doses or medical management with anti-thyroid drugs such as carbimazole. Diffuse uptake is typically consistent with Graves’ Disease and I would perform thyroid antibodies such as TRAb and TPO antibodies. These patients are best managed by collaboration with an Endocrinologist and Endocrine Surgeon.
Stratification of Malignant Risk
The risk of malignancy should always be considered in any thyroid nodule. The risk of malignancy is determined by both sonographic appearance of the nodule and cytology results. Not all thyroid nodules undergo a biopsy (FNA) as a large proportion are benign with the aim of avoiding overdiagnosis and treatment. As a general rule, most thyroid nodules below 1 cm are not biopsied and can be surveyed by ultrasound annually.
The appearance and size of the nodule on sonography are often correlated with a scoring system/guide. The American Thyroid Association (ATA) guidelines and American College of Radiology (ACR-TIRADS) scoring system are the two most commonly used in Australia and New Zealand 2,3. The figures below show the sonographic characteristics that are concerning based on a scoring system (ACR-TIRADS) or risk stratification (ATA) which then determines whether FNA is indicated.
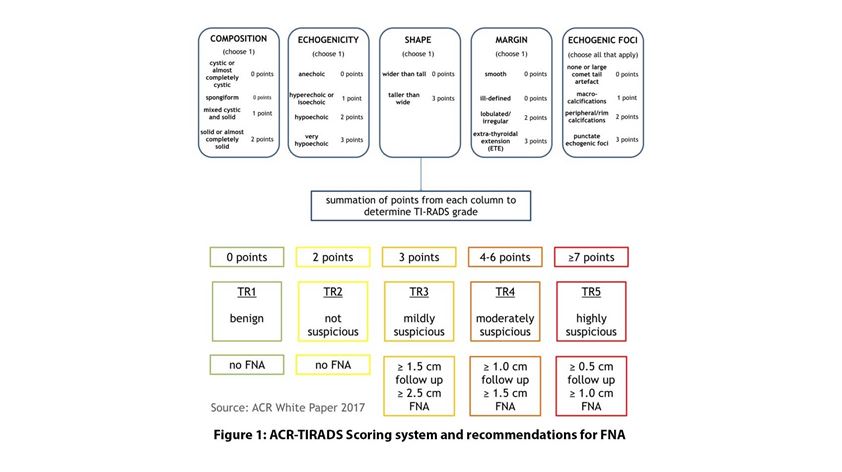
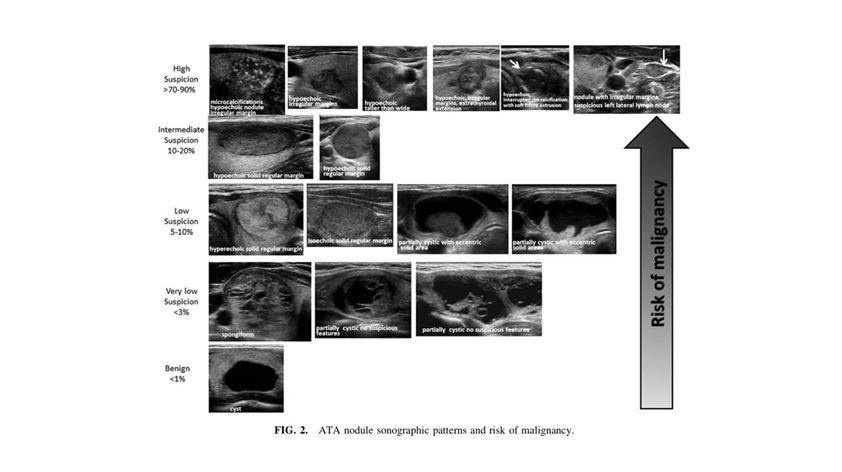
Following the ATA guidelines, a FNA is warranted in all 2
- High suspicion and intermediate suspicion nodules ≥ 1cm
- Low suspicion nodules ≥ 1.5cm
- Very low suspicion nodules ≥ 2cm
- Benign appearing nodules (purely cystic) do not require a biopsy.
Note that there will still be malignant looking thyroid nodules detected on US under 1cm and despite the guidelines these should be assessed by a specialist thyroid surgeon for suitability for observation vs surgical removal based on size and anatomical location in the lobe with respect to the future possibility of extrathyroidal extension, tracheal invasion or recurrent nerve invasion.
What do the biopsy results mean?
Cytological results from the FNA are classified in 6 categories.
- Undiagnostic results typically warrant a repeat sample
- Benign FNA results have a very low risk of malignancy < 1-4% and can be followed up with a serial ultrasound to assess for growth in 12-18 months and a repeat biopsy if there are any further concerning features. Large benign nodules however can often cause compressive symptoms and should be referred for further surgical management if they cannot be aspirated or recur after attempts at aspiration
- Indeterminate/Atypical results carry a 10% risk of malignancy and these patients should be referred to an endocrine surgeon
- A suspicious for follicular neoplasm or hurtle cell neoplasm result carry up to a 20% risk of malignancy and these should always be referred to an Endocrine Surgeon for further management
- A suspicious for malignancy result carries a 60-75% risk of malignancy and should always be referred
- A malignant cytological result is up to 95% accurate; typically papillary thyroid carcinoma and should be referred on for definitive management.
If a targeted ultrasound of the thyroid gland has only been performed in nodules with cytology suspicious for malignancy or malignant nodules, an ultrasound of the neck should also be performed to look for potential lymph node metastasis.
Prof Stan Sidhu
Professor Stan Sidhu is a highly qualified and experienced surgeon specialising in minimally invasive thyroid surgery. Widely respected, he performs over 500 operations every year and is a world renowned academic su

References
1. Jiang H, Tian Y, Yan W, et al. The prevalence of thyroid nodules and an analysis of related lifestyle factors in Beijing communities. Int J Environ Res Public Health. Published online 2016. doi:10.3390/ijerph13040442
2. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. Published online 2016. doi:10.1089/thy.2015.0020
3. Tessler FN, Middleton WD, Grant EG, et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. Published online 2017. doi:10.1016/j.jacr.2017.01.046




