Patient Information Guide Keeping you safe

-
Bedside Handover
Click Here
-
Preventing Pressure Injuries
Click Here
-
Blood Transfusions
Click Here

Reducing the Risk of Infection
We are committed to providing high quality care in a safe and clean environment. Our clinical staff will take every measure to minimise the risk of infection, however, the prevention and control of infection is everyone’s responsibility including staff, doctors, patients and visitors.
Patients and visitors can reduce the risk of infection by:
- Washing hands after going to the bathroom and before eating and using the alcohol-based hand rub when entering and leaving the hospital and patient rooms. This is the single most important action in preventing infection.
- Asking staff to perform hand hygiene if there are concerns this has not been performed.
- Not touching any dressings over drips, lines, tubes or drains inserted in their or their loved one's body.
- Telling a nurse if any wounds, drips, lines, tubes or drains become red, swollen or painful, or if the dressing becomes loose or wet. They will check the site. Drips may need to be removed and replaced on some occasions.
- Keeping the over-bed table and bedside locker uncluttered to assist cleaning staff to access all surfaces. Visitors should also avoid sitting on patients' beds or using patients' bathrooms. Public toilets are available on each floor.
- Covering their mouth and nose with a tissue when they cough or sneeze, or sneeze into your elbow, and clean their hands after with alcohol based hand sanitiser or soap and water.
- Avoiding visiting the hospital if they are feeling unwell (this includes children as well), including cold and flu symptoms and not visiting if they have suffered from any gastroenteritis symptoms for at least 48 hours after symptoms have ceased.

Identification Bands
You will be given an identification band when you're admitted to hospital that will be placed on your wrist or leg which will include your name and date of birth. This will be used as a reference during your stay as a safety check during treatments/procedures, surgery, blood transfusions, specimen collection, and when giving medications.
Make sure to:
- Check the information on the ID band is correct
- Check that you have a red ID band if you have any allergies
- Wear your ID band at all times
Staff will check your ID band before every test or procedure and before giving you any medication. They’ll also ask you what your name is and other details, to make sure that the right patient is getting the right treatment every time. All our hospital staff should be wearing an identification badge. If you can't see their badge, or you're not sure who someone is, please ask.
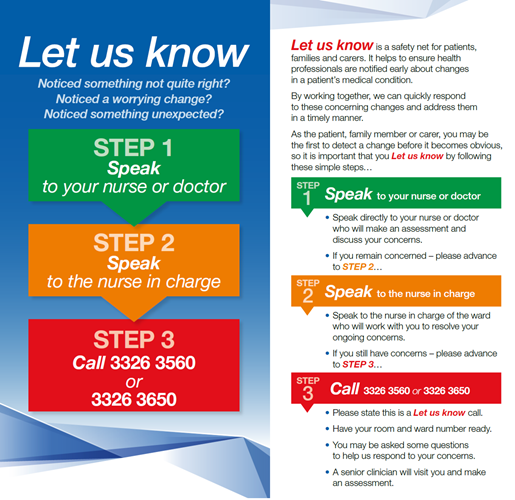
Let Us Know
We understand that you know yourself or your loved one best. This is why we want you to let us know if you notice a worrying change. By working together, we can quickly respond to these concerning changes and address them in a timely manner. Please Let Us Know by following these simple steps:
- Step 1: Speak to your nurse or doctor
- Step 2: Speak to the nurse in charge
- Step 3: Call 07 3326 3560 or 07 3326 3650

Bedside Handover
Clinical handover happens at your bedside at the change of every shift, and if you are being transferred to another ward or department.
We encourage you to get involved and ask questions if there is anything you don’t understand or are concerned about. Your next of kin or carer can also participate in this exchange of information.
Assisting Patients to Move
Our safe handling policy means staff are required to avoid manually lifting patients. We encourage patients to assist in their own movement where possible.
If required, our orderlies will assist you to move and will use handling aids when required for both their and your safety. At times, this may mean there is a delay whilst the proper equipment is being obtained.


Pain Management
Our staff care about your pain. By controlling your pain well during your surgical recovery, you are likely to recover faster and reduce the risk of other complications.
Depending on the nature of your admission, your doctor or anaesthetist may give you options for pain relief. These may include oral tablets, PCA (Patient Controlled Analgesia), and injections. Nurses will regularly ask you to rate your pain on a scale of one to ten (with ten being most painful) and discuss with you the most appropriate form of pain relief.
Your pain should score no more than three or four out of ten. The most important thing you can do is ask for pain relief before you get too uncomfortable or before tasks such as showering or physiotherapy. Frequent, low dose pain relief often provides good control, reducing the need for stronger pain relievers that may have increased side effects. Other options include hot and cold packs, a warm shower and changes of position.

Avoiding Falls
Falls are the most common cause of injury in hospital due to the unfamiliar environment and being physically weaker than usual. Medication changes like pain relief drugs and anaesthetics can also affect your balance. It's important that patients, their family, and staff all work together to reduce the risk of falls.
Patients can reduce their risk of falls whilst in hospital by:
- Bringing their normal walking aids, glasses or hearing aids to hospital and keeping them close to them.
- Making sure they can reach the call bell beside their bed and using it to ask for help as soon as they need it. We’ll strive to answer it immediately but if the ward is busy, it may take a few minutes.
- Wearing supportive, flat, non-slip shoes or slippers. Anti-slip traction socks are also available and should be worn if other suitable footwear is not available.
- Turning the light on so they can see before getting out of bed
- Walking and staying active when family, friends and staff are there to help
- Listening to the advice and recommendations of staff.
- Asking their visitors to let a staff member know when they leave so that they can check on the patient regularly.
Preventing Pressure Injuries
A pressure injury, also known as a bedsore or ulcer, can form when you sit or lie in the same position for a long time. Bony parts of the body like the heels, tailbone, toes, ears and back of your head are at most risk of a pressure injury. Your nurse will perform a risk assessment on admission and review this regularly during your stay. If they feel you are at risk of a pressure injury, they may apply protective dressings to your heels or tailbone.
Patients can prevent a pressure injury by:
- Advising their nurse if they've had previous pressure injuries or slow healing wounds
- Keeping moving and changing their position as often as they can.
- Looking after their skin and advising their nurse if they think it looks or feels different
- Eating a healthy, balanced diet

Preventing Blood Clots
Medication, surgery or being confined to bed can increase your risk of developing a blood clot (Venous Thromboembolism) in your legs or lungs which can be serious. We will regularly assess your risk level for developing a blood clot and help formulate a clot prevention plan. Methods of prevention include medication, anti-thrombolytic stockings (TEDs) and mechanical pump devices for your legs.
Patients can reduce their risk of developing a clot by:
- Taking any tablets or injections that their doctor prescribes
- Keeping their TED stockings on
- Avoiding sitting or lying in bed for long periods, if possible
- Walking as often as their doctor or nurse recommends
- Asking what they can do at home to avoid the risk of a blood clot
Blood Transfusions
If you require a blood transfusion, you will be informed of the reasons, benefits and risks. When you understand and agree to the transfusion, you will be required to sign a consent form.
The procedure involves checking your identification and your observations regularly during administration. If at any time you feel unwell such as hot, itchy, develop a rash, or shortness of breath, let you nurse know immediately.


Medication Safety
Please bring all of the medications that you take with you to hospital including vitamins, herbal medicines such as St Johns Wort, and over-the-counter medications such as Omega 3 and multivitamins.
All medications must be administered to you by a registered/enrolled nurse or doctor. If you are on regular medications, please inform your healthcare team. You may find that some of your normal medicines will not be given during your hospital stay as they may interact with other medications we administer, or procedures and treatments you may be having. Please also inform us during your admission of any allergies or sensitivities you may have.
Please also note that we are unable to administer medications from Webster packs, Dosette boxes or any medications not in their original dispensed packs. If medications are brought to the hospital in this form, new medications will be supplied from the hospital pharmacy. This may result in a cost to the patient depending on their health fund coverage.
To ensure you receive the right medication at the right time, we will always ask for your name, date of birth and if you have any allergies, prior to administering all medications. You can help to further reduce the potential for problems with medications by:
- Asking your healthcare team about any new medications including what they are, what they do, when they are to be taken, and any potential side effects. Become familiar with their names and dosages.
- Making sure the doctors and nurses check your wrist identification band prior to administering medications.
- Telling your healthcare team if you have any concerns or require clarification regarding your medications and treatments.
We will provide you with information, or one of our pharmacists may visit you to discuss any new medications you need to take after discharge.

Delirium
Delirium is a common medical condition that is characterised by fluctuating changes in mental function, occurring more often among older people. It may also be seen in patients following a surgical procedure as well as in those with:
- Illness
- Dementia
- Increasing age (e.g. 70 years or older)
- Depression
- Poor eyesight
- Poor hearing
- Multiple medications (particularly sleeping, pain or psychiatric drugs)
People with delirium show signs of confusion, and may appear either very agitated, quiet or drowsy. The onset of delirium is always sudden. It usually only lasts a few days but may persist for longer periods. Delirium can be a serious condition, but it is usually treatable.
A person with delirium may require special nursing care and closer observation. Family members and carers can provide valuable information to the nurses and doctors caring for the person with delirium. It is important to notify nurses of any sudden changes in a person’s mental or physical condition.
Our goal is to ensure people experiencing delirium are provided a safe environment to optimise healing. Care for patients experiencing delirium may involve:
- Tests to identify the underlying cause of the delirium
- Decreasing stimuli and providing specialised care
- Activities designed to help the person with delirium settle into the hospital environment, e.g. providing fiddle blankets
- In certain situations, and only after other options have been explored, care may also involve use of medications and/or physical aids.
If you have questions about delirium, speak with your doctor or nurse.




