St Vincent's Private Maternity
Frequently Asked Questions
Frequently Asked Questions
If this is your first pregnancy, you probably have lots of questions and it’s hard to know where to look for the right answers. Here are answers to some of the questions most frequently asked by our expectant mothers. If you have other questions, don’t hesitate to call our midwives who will be only too happy to help.
Planning for Pregnancy
No, you don’t need to have private health insurance to give birth in a private maternity hospital. Many mothers choose to be self-funded and pay the full out-of-pocket costs.
If you’re planning to be self-funded, your estimated hospital expenses must be paid on admission. Any additional costs incurred during your stay are payable on discharge.
In Australia, our public hospitals offer a safe and affordable option for pregnancy care and birth. If you choose a public hospital, midwives will look after you during pregnancy and birth. Doctors are on hand to help with any complications.
You may be lucky and get to stay in a private room but many rooms are shared. You’ll normally stay 1 or 2 days.
If you have a Medicare card, most of the costs will be covered.
In a private hospital you’ll have your choice of obstetrician for your pregnancy care and they will attend the birth, as long as they’re available.
Most private hospitals offer well-appointed private rooms with ensuites, room service and other services at no extra cost.
If you are a member of a health fund, it is important to check the following prior to your hospital admission:
1. Your health fund will cover the cost of your obstetric admission and accommodation.
2. How long you have been with your fund? If you have been a member of your health fund for less than 12 months, your fund may not accept liability for the costs of admission.
3. Pharmacy, pathology, imaging and x-rays may attract additional charges. Check if your fund covers any of these.
4. Medical and allied health practitioner fees may be billed separately by the practitioners. These are not included in the estimate from the hospital.
Pregnancy FAQs
Yes, you can exercise and are encouraged to continue exercising except contact sports and very extreme physical exertion. You’ll get more tired more quickly and notice a faster heartbeat which is very normal even in the first trimester when the baby is only a few centimetres in size.
Generally, things that help support and strengthen the core and pelvic floor (such as Pilates or personal training) or moderate cardio or circuit training (with a top heart rate less than 150bpm) are good for you (but chat with your obstetrician or midwife for more tailored advice).
Weight gain during pregnancy is different for everyone, but generally you can expect to put on 10 to 14kg. However, it does depend on your body weight and body mass index (BMI) at the beginning of your pregnancy. If you are underweight, you might be encouraged to gain a bit more. If you are overweight or obese, you might be encouraged to limit your weight gain to 5kg or less.
As your baby grows, it’s normal to gain some weight but it’s important not to gain too much as this can increase your risk of diabetes in pregnancy, high blood pressure and delivery complications. Not gaining enough weight can also have implications. It could increase the risk of premature birth, or cause your baby to be smaller.
Try to focus on healthy eating and staying active while pregnant. Your obstetrician will get you to weigh yourself at each visit, and will talk to you about healthy weight gain. Some mothers are referred by their obstetrician to a specialist dietitian to optimise pregnancy nutrition.
Most of the time, first trimester bleeding is normal and will go away on its own. However, it does cause worry and upset to expecting mothers. Other reasons for first trimester bleeding include miscarriage and sometimes ectopic pregnancy (pregnancy outside the uterus). If you experience bleeding, ask for an appointment with your obstetrician, explaining the situation to the receptionist. Your obstetrician will most likely perform an ultrasound or a blood test.
NIPT is a blood test used to identify pregnancies with an increased chance of having a chromosome condition such as Down syndrome (Trisomy 21), Edward’s syndrome (Trisomy 18) and Patau syndrome (Trisomy 13) as well as sex chromosome abnormalities. You can also find out the sex of the baby by having this test.
NIPT can be performed any time after 10 weeks gestation and is regarded as the most accurate prenatal test to screen for Down’s Syndrome (99%). Your obstetrician will recommend that you still have a 13 week ultrasound to check the early anatomy of the baby, as 40 to 50% of structural abnormalities can be detected at this time and will not be identified on the NIPT blood test alone.
The best position for sleep, especially in the third trimester of pregnancy, is on your side. Research has shown that sleeping on your side at night and for naps is the safest for your baby. In the early part of pregnancy, it’s fine to sleep on your stomach but as your pregnancy progresses, this will become more uncomfortable.
Try not to go to sleep on your back in the third trimester (after 28 weeks). The issue with sleeping on your back is related to the growing pregnant uterus putting pressure on the main vein that returns blood to the heart. This may affect the main blood vessels that supply the uterus, and can potentially restrict blood flow/oxygen to the baby. Lying on your back may also make you feel faint and unwell. If you do wake up on your back in the middle of the night, don’t panic, just turn over onto your side and go back to sleep.
There’s a huge amount of information about Listeria infections out there. Listeria is actually a rare infection and almost always hits the newspapers when there is an outbreak.
Often, the outbreak is in food that’s not commonly on the ‘banned’ list (for instance the recent rockmelon scare). It's not unreasonable to ask yourself; how many tim es have I eaten brie or poached eggs and how often have I got a bad gastro-enteritis from these foods?
The wise course of action is to eat sensibly, avoid take-away and pre-packaged foods that may have been sitting out for long periods of time and be wary particularly of raw, under-cooked or reheated food.
Cytomegalovirus is a virus that’s particularly prevalent in younger children who go to day-care or kindergarten. It is most commonly spread via urine or saliva. A first exposure during pregnancy can cause quite a wide spectrum of problems in the baby up to and including brain damage. It is much more common than Listeria and rarely talked about.
It can be difficult to test for and you are never necessarily immune to cytomegalovirus even if you have had it before. Anyone with a child under the age of 3 or 4, especially if they associate with lots of other children, should assume their child carries cytomegalovirus.
To reduce your risk of getting cytomegalovirus, practice good hand hygiene when exposed to urine (usually nappy changing), and avoid kissing young children on the mouth or sharing food with them while you’re pregnant.
The whooping cough vaccine is very important to have during pregnancy as whooping cough (pertussis) can cause a very serious infection especially in newborns. The vaccination is given to all pregnant women, every time they are pregnant, between 28 and 32 weeks gestation.
This allows time for your body to make antibodies which cross the placenta and provide protection to the baby especially for the early weeks when their immune system is just establishing. This is more effective at reducing the risk of pertussis in young babies compared to waiting and vaccinating after delivery.
We also recommend that family members or friends that are going to have regular close contact with the baby, have the whooping cough vaccine if they have not been vaccinated in the past 5 years.
Yes. Many women want to or need to travel during pregnancy but there a few things to consider. While you are pregnant (and for 6 weeks after delivery) you are at increased risk of deep vein thrombosis (DVT) which is a clot in your calf. Long flights significantly increase this risk. During the flight it’s important that you stay hydrated, move as much as possible (walk up and down the aisle/do leg exercises) and wear compression stockings.
Make sure your travel insurance covers pregnancy in case you become unwell or need to deliver your baby early. It is a good idea to carry documentation of your due date. Your obstetrician will print out your antenatal record for you to take with you. Airlines will allow domestic travel until 36 weeks gestation and travel up to 34 weeks gestation internationally.
When planning overseas travel, you should access the smarttraveller.gov.au website and consider postponing travel to countries where the Zika virus is common. Pregnant women (and women planning a pregnancy) should avoid exposure to the Zika virus as infection during pregnancy may cause severe damage to your unborn baby’s brain development.
Yes! Morning sickness is likely to be at its worst between 6 and 10 weeks and gradually get better between 12 and 20 weeks. It’s very unlikely to persist after 20 weeks. If it is very bad, it is worthwhile getting advice from your obstetrician early in the pregnancy. They can check for things like twins or thyroid disease (which can sometimes be the cause) and can make recommendations on anti-nausea medications.
Labour & Birth FAQs
Pre-labour can last for days of weeks before true labour begins, so how can you tell when it’s really about to happen? When your contractions are getting closer together, stronger and lasting longer it’s time to think about contacting the hospital.
• For your first baby and if you’re between 38 and 42 weeks pregnant, you can wait until the contractions are 5 minutes apart, or they’re getting too painful to manage.
• For your second or subsequent baby, contact the hospital when they’re around 7 minutes apart.
Don’t wait. Contact the midwives straight away if:
• You have having bleeding that’s like a period, rather than just a ‘show’
• Your baby is preterm (under 37 weeks)
• You’ve had a complicated pregnancy
• You previously had a caesarean
• You’re having more than one baby
• Your baby is presenting as a breech (bottom first)
• You can feel pressure in your bowel with a contraction and you feel like pushing
• You had a very rapid previous labour (2-3 hours)
• You have group B strep and need antibiotics in labour
• You’re really worried or not coping
• You live some distance from the hospital, or traffic is likely to slow you down
In Australia, most babies are delivered by vaginal birth. 30% of Australian births are by caesarean section. Your obstetrician will normally recommend a caesarean if they believe there are likely to be problems or risks associated with a vaginal birth.
Sometimes an emergency caesarean is carried out because of pregnancy complications or if your labour doesn't proceed as expected.
Labour is hard work and it hurts. Some women manage to cope with the pain without medical help while others are happy to consider pain relief options. For your first birth, you won’t know whether your pain threshold is high or low, so you might want to consider a range of options. Don’t be afraid to ask for help if you’re not coping.
Non-medical pain relief methods include:
• Staying calm and/or meditating
• Learning breathing techniques
• Support from a trusted partner, friend or doula
• Listening to music
• Hot and cold packs
• Massage
• A warm shower or bath
• Staying active
• Hypnosis
• Acupuncture
• Acupressure
• Transcutaneous electrical nerve stimulation (TENS)
Drug treatment
• Nitrous oxide, known as ‘laughing gas’ can take the edge off your contraction pains. You hold the mask and start breathing it in as a contraction begins.
• Pethidine is an opioid analgesic that provides strong pain relief for up to 4 hours.
• Epidural anaesthesia should make you completely numb from the waist down. It requires an injection into your spine. It is also used for caesarean deliveries.
All drug treatments have potential side effects which you should discuss with your obstetrician.
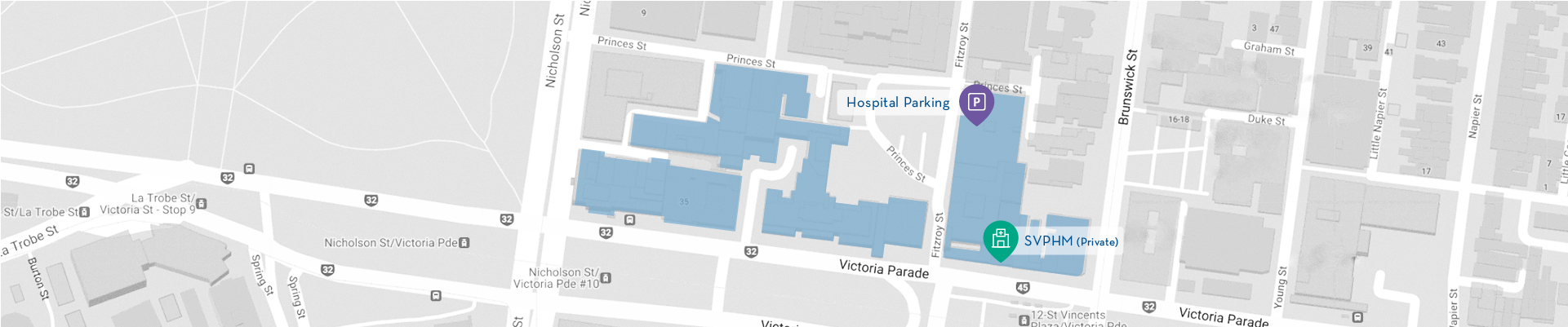
Contact Us